For the past few months, there has been a global spread and toll of COVID-19. So far, humanity has been able to eradicate only one other human infectious disease- smallpox. The novel infectious disease- COVID-19 has had its devastating share of lives globally and currently there is no cure or licensed vaccine.
Many studies lately have been discussing in-depth about neutralizing antibodies. They represent therapeutic and prophylactic options that could help guide potential vaccine designs. Neutralizing antibodies (nAbs) in terms of another respiratory virus- respiratory syncytial virus (RSV) is widely used clinically, usually to protect vulnerable infants prophylactically. Generally, nAbs with good potency also known as super antibodies can supersize antiviral therapeutic efficiency. Along with the help of bioengineering, the nAbs half-life can be prolonged bringing down the cost considerably.
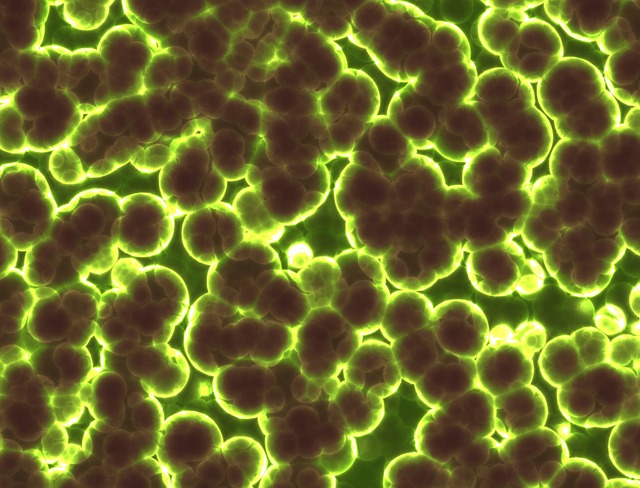
In this study, the authors try to present potent nAbs to the COVID-19 virus and further demonstrate their efficacy in-vivo using small animal models. The researchers of this paper, isolated and characterized the required monoclonal antibodies from recovering convalescent donors and developed neutralizing assays to investigate the antibody responses. In parallel, the researchers also developed both live attenuated and pseudovirus neutralization assays using HeLa- ACE2 (Angiotensin-converting enzyme) cell line. The collected convalescent plasma was evaluated against COVID-19 by using 8 donors. The antigen-specific B cells were sorted and corresponding genes were identified and cloned to enable antibody expression and characterization. The promising monoclonal antibodies were progressed for further testing in-vivo using a small animal model.
The study further isolated the potent neutralizing antibodies to two epitopes- the receptor-binding domain (RBD) and the non RBD- Spike (S) protein. The data showed that the passive transfer of neutralizing antibodies provides distinct protection against the novel- COVID-19 virus as seen in Syrian hamsters. The animal model throughout the infection maintained the same weight and showed low lung abnormalities. Nevertheless, as for any animal model, there were a few limitations, including the difference in receptor cells between the hamster and humans.
The results from the study suggest a focus on the RBD and a string neutralizing antibody responses were seen by immunizing mice with a multivalent RBD. The few weak preponderances of neutralizing antibody to S protein may be due to the result of the study using recombinant S protein. In conclusion, the data from the study potentially open up to the idea of the very rapid generation of neutralizing antibodies to a newly emerged novel virus. The antibodies can open up to the possibilities of finding a clinical application and will aid in vaccine manufacturing or design.