With the number of COVID-19 cases surpassing 4.3 million worldwide and counting, scientists are working around the clock in efforts to develop vaccines and treatments to slow the pandemic. Currently, scientists are looking into whether existing drugs might work or whether new treatments need to be developed to try and tackle the virus.
In this article, we discuss the latest scientific finding, how an antibody identified in a survivor of the 2003 Severe Acute Respiratory Syndrome (SARS) outbreak has the potential to neutralize COVID-19, providing a glimmer of hope in this current battle.
How do these antibodies work against COVID-19?
Development of immunity to a pathogen through natural infection is usually a multi-step process taking around 1-2 weeks. The body immediately reacts to fight the infection with a nonspecific innate response which will slow the progress of the virus and may even prevent it from causing symptoms. This is then followed by an adaptive response where the body produces antibodies specifically binding to the virus and eliminate it along with the cells infected.
Recently a research team came forward and publisher a paper stating that they have identified an antibody from a patient recovered from SARS 2003, which can potentially inhibit the cause of COVID-19. The antibody S309 is now on a fast track development and testing at Vir Biotechnology.
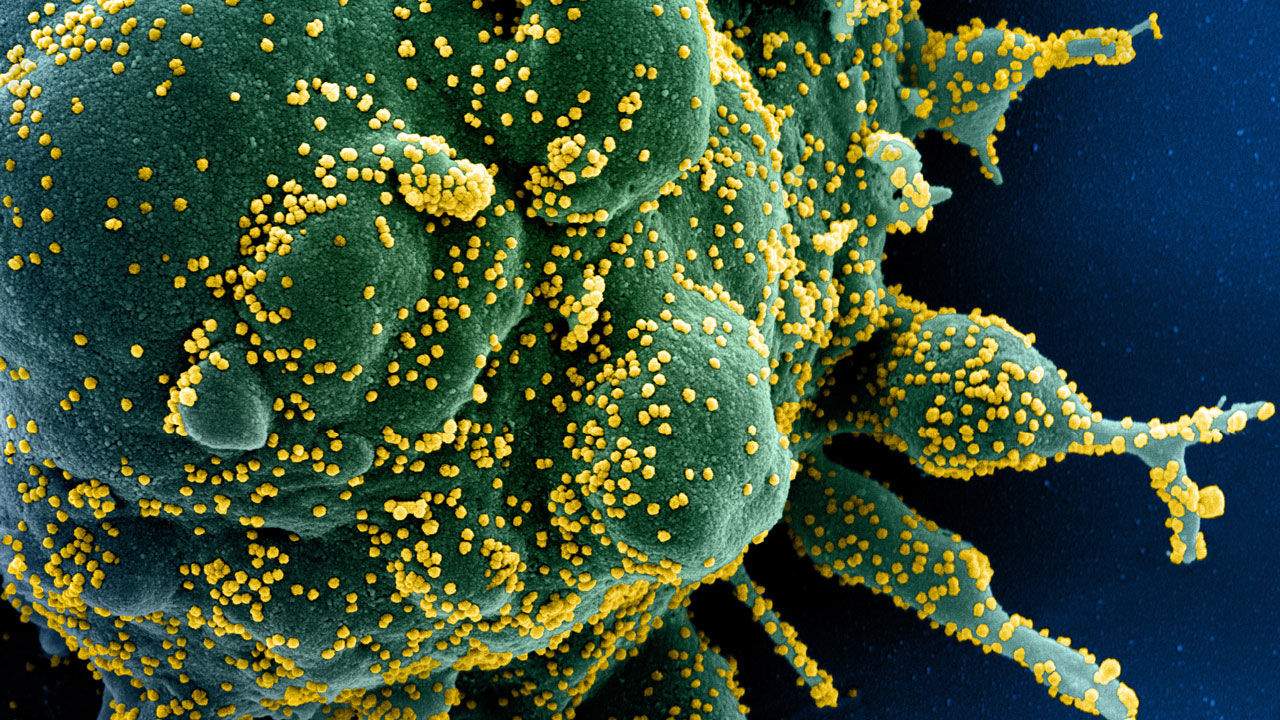
The scientists first identified monoclonal antibodies from the memory B cells of the SARS survivor. The memory B cells reproduce cells and have a long lineage, sometimes for life. The cells have the tendency to remember a pathogen or one similar to it and have the potential to fight against it in the future if re-infected.
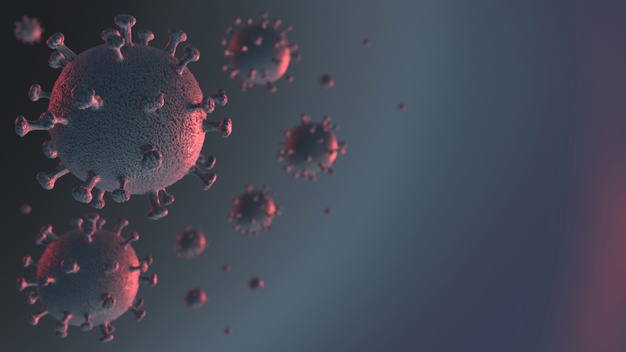
The S309 antibody, in particular, is directed at a protein structure of the coronaviruses. The structure is essential for the virus, to recognize a host cell receptor and infect it. This particular infectivity capability is present in the spikes that crown the virus. S309, in particular, attacks the spike- disabling it, hence hindering the coronavirus to enter the cells. It should also be noted that the antibody showed the capability to target binding sites of several sarbocoviruses, not just COVID-19 and SARS.
What next- Will this be the breakthrough we all are hoping for COVID-19?
In this paper titled “Cross-neutralization of SARS-CoV and SARS-CoV2 by a human monoclonal antibody”, scientists have reported that by combining the S309 antibody with other similar antibodies identified in the recovered SARS survivor, there is a chance of neutralizing the COVID-19 virus. This cocktail of antibodies could be the answer to limit the coronavirus from forming mutants capable of escaping the single ingredient antibody.
“We still need to show that this antibody is protective in living systems, which has not yet been done,” said David Veesler senior author. “Right now there are no approved tools or licensed therapeutics proven to fight against the coronavirus that causes COVID-19”, he added.
At this point in the pandemic, there is not enough evidence to prove the effect of antibody-mediated immunity against the virus. It cannot guarantee an immunity passport or a risk-free certificate. Further research and studies need to be performed before we can reach a conclusion.